Reading an EKG strip is crucial for understanding heart activity. This skill is essential for healthcare professionals, as it aids in diagnosing various cardiac conditions. An EKG Machine displays the electrical impulses of the heart in a graphical format. Familiarity with its components and measurements is necessary for accurate interpretation and effective patient care.
Understanding the Basics of an EKG Strip
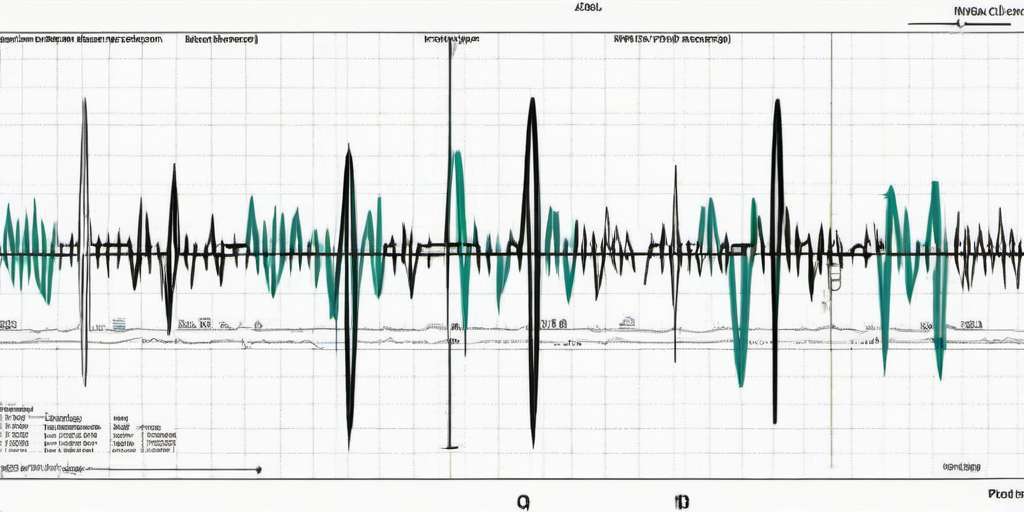
Grasping the fundamentals of an EKG strip is essential for interpreting the heart’s electrical activity effectively. This section explores what an EKG strip represents, its measurements, and its significance in medical practice.
What an EKG Strip Represents
An EKG strip is a graphical representation of the electrical impulses that trigger each heartbeat. These impulses spread across the heart muscle, facilitating coordinated contractions that enable blood circulation. By analyzing the different components of the EKG waveform, healthcare providers can gain crucial insights into the heart’s health and detect potential abnormalities.
EKG Graph Paper and Measurements
Understanding the layout and measurements of EKG graph paper is vital for correct interpretation. The strip is divided into small squares, each of which represents a specific time interval and voltage level.
Horizontal Axis: Time in Seconds
The horizontal axis of the EKG strip indicates time. Each small square typically represents 0.04 seconds, while each large square, which consists of five small squares, represents 0.20 seconds. This time measurement allows clinicians to assess the duration of various components within the EKG waveform.
Vertical Axis: Voltage in Millivolts
The vertical axis indicates the amplitude of the electrical signals measured in millivolts (mV). Each 10 mm representation on the vertical scale equals 1 mV. Understanding the voltage dimensions is necessary for evaluating the strength of the heart’s electrical activity during a cardiac cycle.
Small Boxes and Large Boxes
The EKG graph is constructed using small and large boxes. Recognizing the relationship between these boxes helps in timing and measuring the segments and intervals on the EKG strip. Specifically:
- Each small box measures 1 mm in height and width, representing 0.04 seconds.
- Each large box is made up of 5 small boxes, allowing for a measurement of 0.20 seconds.
Importance of EKG in Medical Practice
The EKG serves as a critical tool in cardiovascular assessment, as it helps detect various heart conditions. Understanding its significance enables healthcare professionals to make informed decisions about patient care.
In clinical settings, EKGs are used to:
- Diagnose arrhythmias, which can lead to serious health complications.
- Monitor the effects of cardiac medications and interventions.
- Identify signs of ischemia, infarction, or other cardiac events.
- Evaluate the overall electrical stability of the heart.
Ultimately, the EKG strip is an indispensable tool for assessing cardiac health and guiding treatment strategies.
Key Components of an EKG Strip
Understanding the key components of an EKG strip is essential for accurate interpretation. Each component represents a specific phase of the heart’s electrical activity, providing crucial information for diagnosing various cardiac conditions.
P-Wave: Atrial Depolarization
The P-Wave signifies the depolarization of the atria, which leads to their contraction. This wave is typically seen before each QRS complex on the EKG strip. The presence of a normal P-Wave indicates that the electrical impulse originates from the sinoatrial (SA) node, synchronizing the heart’s rhythm.
A well-formed P-Wave should be rounded and positive in most leads, measuring no more than 0.12 seconds in duration. Deviations in shape or duration can indicate underlying atrial conditions, such as atrial enlargement or atrial fibrillation.
QRS Complex: Ventricular Depolarization
The QRS complex represents the depolarization of the ventricles, which triggers ventricular contraction. It is a vital feature to assess as it reflects the condition of the ventricular myocardium and the conduction system. Analyzing the QRS complex is crucial for diagnosing various cardiac disorders.
This complex typically lasts between 0.04 and 0.10 seconds. A duration longer than this may suggest a delay in ventricular conduction, while a notably short duration can point to ventricles firing too rapidly.
Measuring the QRS Complex
To measure the QRS complex, one must identify the start of the Q wave and the end of the S wave. The duration is recorded in seconds and converted into the appropriate measure on the EKG graph paper. Any prolonged or altered QRS interval requires further investigation, as it might indicate underlying cardiac problems, such as bundle branch block or myocardial infarction.
T-Wave: Ventricular Repolarization
The T-wave follows the QRS complex and indicates the repolarization of the ventricles. During this phase, the cardiac muscle cells prepare for the next contraction. The T-wave shape provides insights into the heart’s recovery period following ventricular contraction.
Normally, the T-wave is rounded and primarily positive in shape. In certain conditions, such as ischemia or electrolyte imbalances, the T-wave can become inverted or flattened, signifying potential underlying issues needing clinical attention.
PR Interval: Conduction Time
The PR interval represents the time taken for the electrical impulse to travel from the atria to the ventricles. This interval includes the P-Wave and the flat line (isoelectric line) following it until the QRS complex begins. A normal PR interval ranges from 0.12 to 0.20 seconds.
If the PR interval is prolonged, it may indicate a block in the electrical conduction system, known as atrioventricular (AV) block. Conversely, a shortened PR interval might suggest conditions such as Wolff-Parkinson-White syndrome, where accessory pathways exist.
ST Segment: Ventricular Plateau Phase
The ST segment follows the QRS complex and represents the period when the ventricles are depolarized and are in a plateau phase. During this critical moment, the heart muscle contracts and begins to prepare for repolarization, stabilizing the electrical activity before the next heartbeat.
The ST segment should appear flat on the EKG. Any elevation or depression in the ST segment may indicate myocardial ischemia or infarction, necessitating immediate clinical evaluation.
QT Interval: Total Ventricular Activity
The QT interval measures the total time taken for the ventricles to depolarize and then repolarize, effectively capturing the entire electrical cycle of the ventricular myocardium. It extends from the beginning of the Q wave to the end of the T wave. A normal QT interval ranges from 0.35 to 0.44 seconds, depending on the heart rate.
A prolonged QT interval can predispose patients to life-threatening arrhythmias such as Torsades de Pointes. Factors such as electrolyte imbalances, medications, and genetic predispositions often contribute to QT prolongation, warranting thorough assessment and management.
Steps for Reading an EKG Strip
Understanding how to interpret an EKG strip involves a systematic approach that focuses on various elements. This method ensures accurate readings and aids in diagnosing potential cardiac issues.
Evaluating Heart Rhythm Regularity
The first step in reading an EKG strip is to assess the regularity of the heart rhythm. This involves examining the intervals between the R waves.
Identifying the Rhythm
A clear identification of the rhythm is critical. This can be determined by measuring the intervals between R-R peaks. A regular rhythm will show consistent R-R intervals, while an irregular rhythm may vary in duration, indicating potential arrhythmias.
Calculating Heart Rate
Once the rhythm has been evaluated, calculating the heart rate is the next essential step. Understanding both regular and irregular rhythms is crucial for accurate readings.
Number of Large Squares Method
For a regular rhythm, the heart rate can be calculated using the number of large squares between two consecutive R waves:
- Count the number of large squares between R waves.
- Divide 300 by this number to find the beats per minute (BPM).
Six-Second Strip Method
For irregular rhythms, the six-second strip method can be utilized:
- Count the number of R waves in a six-second interval.
- Multiply this number by 10 to determine the heart rate.
Identifying and Analyzing P-Waves
Identifying P-waves is crucial as they represent atrial depolarization. These waves should precede each QRS complex and have a consistent morphology.
Measuring PR Interval
The PR interval is measured from the beginning of the P-wave to the start of the QRS complex. A normal PR interval ranges from 0.12 to 0.20 seconds. Prolongation of this interval may indicate potential conduction delays.
Measuring QRS Complex Duration
The duration of the QRS complex is pivotal as it reflects ventricular depolarization. Measuring from the start to the end of the QRS, the normal range is between 0.04 and 0.10 seconds. A longer duration may suggest a bundle branch block or other disturbances in conduction.
Assessing T-Wave Morphology
The T-wave indicates ventricular repolarization. Evaluating its shape and orientation is essential. A normal T-wave is generally upright and symmetrical. Abnormalities may suggest issues like ischemia or electrolyte imbalances.
Detecting ST Segment Deviations
The ST segment occurs after the QRS complex and reflects the period of ventricular depolarization. Elevation or depression of the ST segment can indicate significant health concerns, including myocardial ischemia or infarction.
Identifying Abnormal Beats
Lastly, identifying abnormal beats is key when analyzing an EKG strip. This may include:
- Premature Atrial Contractions (PACs)
- Premature Ventricular Contractions (PVCs)
- Other ectopic beats that deviate from the normal rhythm
Recognizing these anomalies requires careful observation and a comprehensive understanding of normal versus abnormal patterns.
Common EKG Findings and Their Interpretation
Understanding common EKG findings is crucial for accurate interpretation. Each finding can indicate different cardiac conditions, making it essential for healthcare professionals to recognize and analyze them effectively.
Normal Sinus Rhythm
Normal sinus rhythm (NSR) is characterized by a consistent heart rate of 60 to 100 beats per minute, originating from the sinoatrial node. The EKG shows a regular pattern with equal intervals between R-R intervals. Each P-Wave precedes the QRS complex, indicating proper atrial contraction. The PR interval should remain within 0.12 to 0.20 seconds, and the QRS complex typically lasts between 0.04 and 0.10 seconds.
Atrial Fibrillation and Flutter
Atrial fibrillation (AF) presents as an irregularly irregular rhythm with no distinct P-Waves, indicating chaotic electrical activity in the atria. The heart rate may be fast or slow. In contrast, atrial flutter appears as a “sawtooth” pattern known as “F-waves,” commonly seen in inferior leads. Treatment often focuses on controlling heart rate and reducing the risk of thromboembolic events.
Premature Atrial and Ventricular Contractions
Premature contractions can arise from either the atria or the ventricles. Premature atrial contractions (PACs) are characterized by an early P-Wave and a compensatory pause following the early beat. In contrast, premature ventricular contractions (PVCs) show a wide and bizarre QRS complex without a preceding P-Wave. Frequent occurrences may indicate underlying pathology and should be evaluated further.
Bradycardia and Tachycardia
Bradycardia refers to a heart rate of fewer than 60 beats per minute and can be associated with healthy athletes or pathological conditions such as heart block. Tachycardia, on the other hand, indicates a heart rate exceeding 100 beats per minute, which can arise from various factors, including stress, fever, or cardiac anomalies.
Ventricular Tachycardia and Fibrillation
Ventricular tachycardia (VT) presents as three or more consecutive PVCs at a rapid rate, with potentially life-threatening implications. Its appearance on an EKG can vary but generally shows a uniform QRS complex. Ventricular fibrillation (VF), however, appears as chaotic and disorganized electrical activity, resulting in ineffective contractions and requiring immediate medical intervention.
Myocardial Infarction Indicators
Myocardial infarction (MI) indicators on an EKG include ST-segment elevation or depression, T-Wave inversions, and the presence of abnormal Q waves. ST-segment elevation is indicative of an acute myocardial infarction and is characterized by an upward shift from the baseline. Conversely, ST-segment depression may reflect ischemia, and the presence of significant Q waves can suggest a previous heart attack.
Practice with EKG Strips
Practicing with EKG strips is crucial for developing proficiency in EKG interpretation. Regular practice enables healthcare professionals to identify patterns, recognize abnormalities, and enhance diagnostic skills effectively.
EKG Strip Practice Tests
Practice tests serve as valuable tools for honing EKG reading skills. These tests typically include a variety of EKG strips that vary in complexity, providing opportunities to analyze different cardiac rhythms and conditions.
- Practice tests should include strips with common and uncommon findings.
- Tests can help reinforce knowledge about rhythm recognition and measurement calculations.
- Reviewing answers post-assessment is essential for understanding mistakes and improving technique.
Reviewing Practice EKG Strips
Reviewing previously analyzed EKG strips is beneficial for reinforcing learned concepts and refining technical skills. This process involves carefully going over each component present in the strip and drawing connections to cardiological implications.
- Identify each wave and segment present in the strip.
- Correlate findings to known clinical scenarios to enhance understanding.
- Discuss findings with peers or mentors to gain different perspectives on interpretation.
Common Mistakes and How to Avoid Them
In EKG interpretation, certain mistakes often occur that can lead to misdiagnoses. Recognizing these errors is vital for improving accuracy. Common pitfalls include miscalculating intervals, overlooking waveforms, and misinterpreting abnormal findings.
- Ensure proper measurement of PR intervals and the QRS complex to avoid misdiagnosis.
- Double-check the presence of P-waves in relation to QRS complexes to identify rhythm irregularities.
- Practice a systematic approach to reviewing EKGs, which can help mitigate oversight.
Advanced Interpretation Techniques
Advanced interpretation techniques for EKG strips allow healthcare professionals to uncover intricate details underlying the heart’s electrical activity. These techniques enhance diagnostic accuracy and enable better patient management.
Axis Determination
Axis determination refers to identifying the direction of the heart’s electrical activity throughout the cardiac cycle. It is crucial for diagnosing various cardiac conditions, including ventricular hypertrophy and bundle branch blocks.
To determine the axis, practitioners analyze the QRS complexes in the frontal plane leads (I, II, III, aVR, aVL, aVF). The net positive or negative deflection of these leads provides insights into the electrical orientation of the heart. Each lead corresponds to a specific angle:
- Lead I: 0 degrees
- Lead II: +60 degrees
- Lead III: +120 degrees
- aVR: -150 degrees
- aVL: -30 degrees
- aVF: +90 degrees
By constructing a hexaxial reference system, clinicians can visualize the axis and easily identify deviations from the normal range, such as left axis deviation or right axis deviation, which may signal underlying heart pathology.
Bundle Branch Blocks
Bundle branch blocks (BBB) occur when there is a delay in electrical conduction through the right or left bundle branches of the heart’s conduction system. EKG examination offers direct insights into these abnormalities, often visible in the QRS complex morphology.
There are two primary types of bundle branch blocks:
- Right Bundle Branch Block (RBBB): Characterized by a widened QRS complex (greater than 0.12 seconds) and an “M”-shaped appearance in leads V1 and V2.
- Left Bundle Branch Block (LBBB): Also manifests with a widened QRS complex, with a characteristic “W”-shaped pattern in leads V5 and V6 and typically absence of a Q wave in lead I.
Recognition of bundle branch blocks is vital, as they can indicate underlying cardiac disease or dysfunction. Understanding the type of block can guide further diagnostic testing and management approaches.
Identifying Hypertrophy Patterns
Identifying hypertrophy patterns involves assessing the EKG strip for signs of cardiac muscle thickening, often due to chronic pressure overload or volume overload. Commonly associated with hypertension or valvular heart disease, detecting hypertrophy is important for treatment planning.
The most recognized criteria for left ventricular hypertrophy (LVH) and right ventricular hypertrophy (RVH) are as follows:
- Left Ventricular Hypertrophy: Criteria include a deep S wave in V1 combined with a tall R wave in V5 or V6 with a sum greater than 35 mm, or a more than 20 mm R wave in lead I.
- Right Ventricular Hypertrophy: Identified by a dominant R wave in lead V1 with a height exceeding 7 mm, often accompanied by right axis deviation.
Hypertrophy patterns are visual indicators of the heart’s structural adaptation to increased workload. Recognizing these patterns assists healthcare providers in making informed decisions regarding management and further investigations.
Clinical Correlation and Patient Management
Understanding the relationship between EKG findings and clinical symptoms is crucial for effective patient management. Accurate interpretation of EKG strips allows healthcare professionals to correlate cardiac activity with the patient’s condition and devise appropriate treatment strategies.
Integrating EKG Findings with Clinical Symptoms
To ensure optimal patient care, it’s imperative to connect the dots between EKG results and clinical presentations. This integration involves:
- Evaluating presenting symptoms such as chest pain, shortness of breath, or palpitations to determine the clinical urgency.
- Assessing risk factors, including history of cardiac disease, diabetes, hypertension, or family history of heart problems.
- Considering physical examination findings that may indicate heart dysfunction, like murmur or abnormal heart sounds.
- Cross-referencing EKG changes with laboratory results, such as cardiac biomarkers, to confirm diagnoses like myocardial infarction or heart failure.
For instance, an EKG strip showing ST-segment elevation demands immediate action in a patient exhibiting acute chest pain. Conversely, a normal sinus rhythm in a patient with fatigue may redirect the clinician’s focus to non-cardiac causes.
Case Studies and Real-World Examples
Analyzing real-world cases can elucidate the practical application of EKG interpretation in clinical settings. Examples include:
- A 65-year-old male with acute chest pain and an EKG displaying ST-segment elevation indicating a myocardial infarction, leading to prompt treatment.
- A 45-year-old female presenting with palpitations, where EKG findings revealed atrial fibrillation. Management entailed rate control and anticoagulation to reduce stroke risk.
- A young athlete experiencing syncope, prompting an EKG that uncovered Brugada syndrome, necessitating lifestyle changes and possible implantable devices.
These scenarios represent the diversity of patient presentations requiring EKG analysis, highlighting the importance of clinical context in decision-making.
Collaborating with Healthcare Teams
Effective management of patients with EKG abnormalities often requires a team approach. Collaboration among healthcare professionals is vital for:
- Sharing insights on EKG interpretations among nurses, physicians, and cardiologists to ensure comprehensive patient assessments.
- Developing coordinated treatment plans that consider all aspects of a patient’s health status, including non-cardiac issues that could affect cardiac function.
- Engaging in multidisciplinary discussions during case reviews to foster continuous learning and improvement in EKG interpretation skills.
- Implementing protocols for timely intervention in acute cases, leveraging the expertise of various team members, including emergency medical technicians when necessary.
By working collaboratively, healthcare teams can optimize patient outcomes through collective knowledge and shared decision-making, ultimately enhancing care quality.
Tools and Resources for EKG Interpretation
Having access to the right tools and resources is crucial for mastering EKG interpretation. These resources enhance knowledge, improve accuracy, and foster continuous learning among healthcare professionals.
EKG Interpretation Software
Advanced software solutions are available that assist in the analysis and interpretation of EKG data. These programs often come equipped with features that enhance the user’s ability to read and analyze EKG strips effectively. Key functionalities typically include:
- Automated rhythm analysis to identify abnormalities
- Integration of patient data for comprehensive assessments
- Comparison tools to evaluate past and present EKGs
- Support for various EKG lead configurations
- Customizable reporting features for documenting findings
Such software can significantly aid in reducing interpretation errors and improving patient outcomes. However, reliance solely on software without clinical judgment can lead to oversights, so it is important for users to maintain a fundamental understanding of EKG principles.
Continuing Medical Education
Continuous education is essential for healthcare professionals. Engaging in ongoing training helps refine EKG interpretation skills and stay updated on the latest developments in cardiology. Various avenues exist for pursuing continuing education:
- Online courses and webinars that cover specific aspects of EKG interpretation.
- Workshops and seminars offered by professional organizations and medical institutions.
- Cme programs that provide credits and enhance professional qualifications.
- Conferences focusing on cardiology, where workshops often include hands-on EKG interpretation sessions.
These educational resources not only deepen understanding but also facilitate networking opportunities with other professionals in the field.
Recommended Reading and Online Resources
A wealth of literature and online materials provide valuable information about EKG interpretation. Resources range from textbooks to articles, each offering insights into various aspects of cardiac health. Recommended reading includes:
- Textbooks that cover basic to advanced EKG interpretation concepts.
- Peer-reviewed journals that publish recent findings and case studies.
- Online platforms that provide case simulations and quizzes for practical learning.
- Video tutorials that visually explain complex concepts and techniques.
Utilizing these resources can enhance expertise and help in staying informed about current best practices in the field of cardiology.
Citations:
https://nurse.org/articles/how-to-read-an-ECG-or-EKG-electrocardiogram
http://www.meddean.luc.edu/lumen/meded/medicine/skills/ekg/les1prnt.htm

